Abstract
Background: Sickle cell disease (SCD) is a major public health problem in Sub-Saharan Africa, which is home to about 70% of the affected individuals worldwide. Pregnancy is an emerging life-threatening complication of SCD with high rates of sickle cell specific, maternal and perinatal complications. In low-resource countries, pregnancy in women with SCD is associated with a 22-fold risk of death compared to those without SCD. Perinatal mortality rates are also increased by nearly four-fold.[ BJOG: An International Journal of Obstetrics & Gynaecology. 2016 Apr;123(5), 691-698 ] Preliminary data showed that maternal mortality ratio among pregnant women with and without SCD, at Korle-Bu Teaching Hospital, in Ghana, were 10,791 and 540 per 100,000 live births, respectively. In 2015, we created a multi-disciplinary care team including: obstetricians, hematologists, anesthesiologists with training in pulmonary medicine, pediatricians and midwives to provide care in a combined clinic visit during pregnancy for maternal and fetal surveillance. In a prior before and after study design, we demonstrated a 90% reduction in maternal mortality in SCD after instituting a combined obstetrics and SCD clinic. The odds ratio for maternal mortality in women with and without SCD is similar in high-income countries but discordant in low-income countries. The difference suggests modifiable risk factors contribute to mortalities in the latter setting. We tested the hypothesis that a combined obstetrics and SCD clinic would decrease the mortality rate in pregnant women with SCD living in a low-resource setting.
Methods: In a prospective study, pregnant women with SCD and their parity-matched non-SCD controls were enrolled from their first antenatal visit, through labor and delivery and followed until six weeks postpartum. All participants were reviewed at combined obstetrics and SCD clinic and the following care were standardized: pulse oximeters were used to measure oxygen saturation at baseline and during hospitalizations for acute pain; latex balloons were used for routine incentive spirometry during acute pain episode and post-cesarean section; two wards were designated for the participants for effective management; critically ill patients were discussed by a multi-disciplinary care team including an obstetrician, hematologist, and anesthesiologist. The primary outcome of our study was maternal mortality, defined as the death of a woman while pregnant and up to 42 days after termination of pregnancy from a cause related to or aggravated by the pregnancy or its management irrespective of the site and duration of the pregnancy but excluding incidental causes. Autopsy was performed by a pathologist to identify the cause of death. Antepartum admissions rate, pain and acute chest syndrome rates, preeclampsia, type of delivery and perinatal outcomes were compared between cohorts. Negative binomial regression was used to predict factors associated with adverse outcome. The risk was expressed as relative risk (RR) at 95% confidence interval (95% CI) with significance at p<0.05.
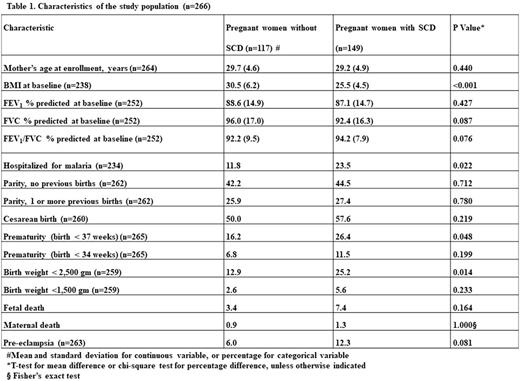
Results: A total of 149 pregnant women with SCD (HbSS=54, HbSC=95) and 113 without SCD were included in the analysis. The mean age [29.2yrs vrs 29.7yrs, p=0.440] and parity [nulliparous 44.5% vrs42.2%, p=0.704] of the two groups were similar. Participants with SCD had a lower BMI at enrollment [BMI 25.5 kg/m2 vs 30.5kg/m2,p<0.001]. Maternal (1.3% vrs 0.9% p=1.00) and perinatal (7.4% vrs 3.4% p=0.164) death rates were similar between the two groups. Pregnant women with SCD had a higher incidence of hospitalization for malaria (23.5% vrs 11.4% p=0.022), preterm birth less than 37 weeks (26.4% vrs 16.2%, p=0.048) and low birth weight (<2500g) (25.2% vrs 12.9% p=0.014) than those without SCD. In a multivariable logistic regression model, SCD was associated with a 4-fold increased risk of preeclampsia when compared to women without SCD (RR 4.487 95%CI 1.501 - 10.517, p = 0.002).
Conclusion: Multi-disciplinary care of pregnant women with SCD in a combined obstetrics and sickle cell disease clinic resulted in similar maternal and perinatal death rates between women with SCD and those without SCD in low-resource setting. Pregnant women with SCD have a significantly higher risk of preeclampsia and premature delivery. Interventions for preeclampsia in women with SCD should be considered in a systematic manner.
Oppong: Office of Research Innovation and Development (ORID) Research Fund/8/LMG-008, University of Ghana; Doris Duke Charitable Foundation; Burroughs Wellcome Foundation; Phillips Family Donation; Aaron Ardoin Foundation for Sickle Cell Anemia; Vanderbilt Univer: Research Funding. Olayemi: Office of Research Innovation and Development (ORID) Research Fund/8/LMG-008, University of Ghana; Doris Duke Charitable Foundation; Burroughs Wellcome Foundation; Phillips Family Donation; Aaron Ardoin Foundation for Sickle Cell Anemia; Vanderbilt Univer: Research Funding. Adomakoh: Office of Research Innovation and Development (ORID) Research Fund/8/LMG-008, University of Ghana; Doris Duke Charitable Foundation; Burroughs Wellcome Foundation; Phillips Family Donation; Aaron Ardoin Foundation for Sickle Cell Anemia; Vanderbilt Univer: Research Funding. Asare: Office of Research Innovation and Development (ORID) Research Fund/8/LMG-008, University of Ghana; Doris Duke Charitable Foundation; Burroughs Wellcome Foundation; Phillips Family Donation; Aaron Ardoin Foundation for Sickle Cell Anemia; Vanderbilt Univer: Research Funding. Mensah: Office of Research Innovation and Development (ORID) Research Fund/8/LMG-008, University of Ghana; Doris Duke Charitable Foundation; Burroughs Wellcome Foundation; Phillips Family Donation; Aaron Ardoin Foundation for Sickle Cell Anemia; Vanderbilt Univer: Research Funding. Swarray-Deen: Office of Research Innovation and Development (ORID) Research Fund/8/LMG-008, University of Ghana; Doris Duke Charitable Foundation; Burroughs Wellcome Foundation; Phillips Family Donation; Aaron Ardoin Foundation for Sickle Cell Anemia; Vanderbilt Univer: Research Funding. Osei-Bonsu: Office of Research Innovation and Development (ORID) Research Fund/8/LMG-008, University of Ghana; Doris Duke Charitable Foundation; Burroughs Wellcome Foundation; Phillips Family Donation; Aaron Ardoin Foundation for Sickle Cell Anemia; Vanderbilt Univer: Research Funding. Crabbe: Office of Research Innovation and Development (ORID) Research Fund/8/LMG-008, University of Ghana; Doris Duke Charitable Foundation; Burroughs Wellcome Foundation; Phillips Family Donation; Aaron Ardoin Foundation for Sickle Cell Anemia; Vanderbilt Univer: Research Funding. Musah: Office of Research Innovation and Development (ORID) Research Fund/8/LMG-008, University of Ghana; Doris Duke Charitable Foundation; Burroughs Wellcome Foundation; Phillips Family Donation; Aaron Ardoin Foundation for Sickle Cell Anemia; Vanderbilt Univer: Research Funding. Boafor: Office of Research Innovation and Development (ORID) Research Fund/8/LMG-008, University of Ghana; Doris Duke Charitable Foundation; Burroughs Wellcome Foundation; Phillips Family Donation; Aaron Ardoin Foundation for Sickle Cell Anemia; Vanderbilt Univer: Research Funding. Rodeghier: Rodeghier consultants: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal